The liver's internal clock has long been recognized as a master conductor of metabolic processes, but recent research reveals far more sophisticated mechanisms than previously understood. Scientists have uncovered how hepatocytes dynamically reorganize their metabolic functions in response to circadian signals, creating waves of enzymatic activity that ripple through biochemical pathways. This discovery fundamentally changes our perspective on how organs "tell time" and use this information to optimize physiological function.
At the core of this regulatory system lies a remarkable synchronization between nuclear receptor proteins and mitochondrial activity. Researchers observed that certain nuclear receptors in liver cells undergo circadian phosphorylation, which alters their ability to bind to metabolic gene promoters. This post-translational modification creates a metabolic "memory" that persists even when the core clock machinery is disrupted, suggesting an elegant fail-safe mechanism evolved to maintain metabolic homeostasis.
The mitochondrial connection has proven particularly fascinating. Hepatic mitochondria don't merely respond to circadian signals - they actively participate in timekeeping. Through rhythmic fluctuations in membrane potential and reactive oxygen species production, these powerhouses of the cell provide feedback that reinforces the central circadian rhythm. This bidirectional communication between nuclear and mitochondrial clocks creates a robust system for anticipating and responding to daily fluctuations in nutrient availability.
Emerging evidence points to an unexpected role for hepatic stellate cells in this chronometabolic regulation. Once considered mere vitamin A storage units, these star-shaped cells have been found to secrete circadian-regulated factors that influence hepatocyte metabolism. The stellate cell-hepatocyte cross-talk appears particularly important for timing lipid processing, with disruption of this communication leading to metabolic dysfunction despite normal hepatocyte clocks.
Metabolic compartmentalization across the liver lobule adds another layer of complexity. Scientists have identified distinct circadian programs operating in periportal versus pericentral hepatocytes, allowing the liver to spatially segregate metabolic processes according to time of day. This zonation creates what researchers describe as a "metabolic conveyor belt" that moves substrates through different biochemical pathways as they flow from the portal triad to the central vein.
The implications for metabolic disease are profound. Studies in shift workers and jet-lagged mice reveal that circadian misalignment doesn't simply disrupt sleep - it reprograms entire metabolic networks. The liver appears particularly vulnerable, with mistimed feeding leading to inappropriate activation of lipogenic pathways during what should be a catabolic phase. This may explain why chronic circadian disruption so frequently leads to fatty liver disease independent of caloric intake.
Intriguingly, the liver's circadian metabolic regulation extends beyond classical clock genes. Researchers identified a novel class of circadian-regulated microRNAs that fine-tune metabolic enzyme expression without directly involving the core clock machinery. These "metabolic microRNAs" appear to serve as a secondary timekeeping system that buffers against perturbations in the primary circadian oscillator.
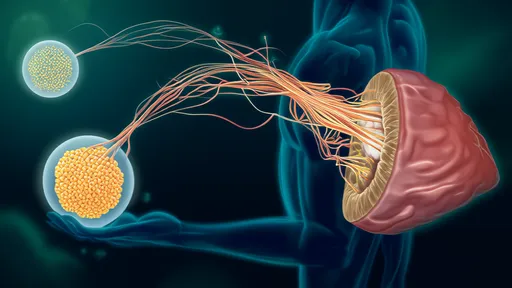
The gut-liver axis plays a surprisingly important role in hepatic circadian metabolism. Microbial metabolites like secondary bile acids and short-chain fatty acids have been shown to entrain peripheral clocks in the liver, creating a feedback loop where diet shapes circadian rhythms which in turn regulate metabolic responses to that diet. This may explain why time-restricted feeding shows such promise for metabolic health - it synchronizes these interconnected systems.
Technological advances have been crucial in these discoveries. The development of real-time metabolomics in freely moving animals has revealed ultradian metabolic rhythms superimposed on circadian cycles. These higher-frequency oscillations suggest the existence of previously unrecognized "metabolic gears" that allow the liver to rapidly adjust its function in response to changing conditions while maintaining overall circadian coherence.
Perhaps most surprisingly, the liver's circadian program appears to influence systemic aging processes. Studies in progeroid mice show that restoring hepatic circadian function can ameliorate multiple aging-related metabolic defects, even when circadian disruption persists in other tissues. This positions the liver as both a victim and perpetrator in the metabolic decline associated with aging and circadian dysfunction.
These findings collectively paint a picture of the liver not as a passive follower of central circadian commands, but as an active participant in a distributed timing network. The organ integrates signals from multiple sources - neural, hormonal, microbial, and metabolic - to create a dynamic, self-correcting metabolic program exquisitely tuned to both internal time and external conditions.
As research continues, scientists are beginning to appreciate how pharmaceutical treatments might be optimized by considering hepatic circadian rhythms. Already, studies show that timing medication administration to coincide with peak expression of drug-metabolizing enzymes can dramatically alter efficacy and toxicity profiles. The emerging field of chronopharmacology may soon transform how we approach metabolic disorders.
The complexity of the liver's circadian metabolic regulation continues to surprise researchers. What began as simple observations of daily enzyme fluctuations has blossomed into the recognition of an entire temporal dimension to metabolism - one that we are only beginning to understand and appreciate. As this field progresses, it promises to rewrite textbooks on both chronobiology and metabolic regulation.
The scientific community has long been fascinated by the intricate relationship between intermittent fasting and cellular autophagy. Recent breakthroughs in metabolic research have shed new light on the precise fasting durations required to trigger this vital cellular recycling process. As laboratories worldwide race to decode the molecular mechanisms behind these findings, we stand at the precipice of potentially revolutionary health applications.
In recent years, the study of myokines—bioactive molecules secreted by skeletal muscle—has revolutionized our understanding of how muscle tissue communicates with distant organs to regulate metabolic homeostasis. Once considered merely a contractile organ, skeletal muscle is now recognized as a potent endocrine organ capable of influencing systemic glucose and lipid metabolism through the secretion of these muscle-derived factors. Researchers are uncovering intricate pathways by which myokines modulate energy balance, offering new therapeutic avenues for metabolic disorders such as diabetes and obesity.
The liver's internal clock has long been recognized as a master conductor of metabolic processes, but recent research reveals far more sophisticated mechanisms than previously understood. Scientists have uncovered how hepatocytes dynamically reorganize their metabolic functions in response to circadian signals, creating waves of enzymatic activity that ripple through biochemical pathways. This discovery fundamentally changes our perspective on how organs "tell time" and use this information to optimize physiological function.
The gradual decline of mitochondrial function has emerged as a cornerstone in understanding the biology of aging and age-related diseases. Once considered mere cellular powerplants, mitochondria are now recognized as dynamic signaling hubs that influence metabolism, redox balance, and cell fate decisions. As research peels back the layers of mitochondrial complexity, scientists are uncovering compelling evidence that early interventions could potentially delay or mitigate multiple aspects of physiological decline.
The field of mental health treatment has undergone a quiet revolution in recent years, with virtual reality (VR) therapy emerging as a powerful clinical tool. What began as an experimental approach in research labs has now entered mainstream therapeutic practice, offering new hope for patients with conditions ranging from phobias to PTSD. Unlike traditional talk therapy or medication-based approaches, VR therapy creates immersive, controlled environments where patients can confront and process their challenges in real-time.
For decades, healthcare providers have grappled with the challenge of medication adherence. Patients forgetting to take their pills, misunderstanding dosage instructions, or simply abandoning treatment plans have long been roadblocks to effective care. The consequences are staggering—studies suggest that poor medication adherence leads to approximately 125,000 preventable deaths annually in the United States alone, not to mention billions in avoidable healthcare costs. But a quiet revolution is underway in the form of smart pillboxes, and early research suggests these unassuming devices might hold the key to solving one of healthcare's most persistent problems.
In an era where health tracking apps have become ubiquitous, the conversation around privacy protections has taken center stage. These applications collect vast amounts of sensitive data, from heart rate readings to sleep patterns, creating a treasure trove of personal information. The way companies handle this data is under increasing scrutiny from both users and regulators alike.
The digital transformation of healthcare has brought unprecedented convenience to medical services, yet it has also introduced complex security challenges surrounding electronic health records (EHRs). As sensitive patient data migrates from paper folders to cloud servers, the stakes for protecting this information have never been higher. Healthcare organizations globally are grappling with how to balance accessibility with robust security measures in an era where cyber threats grow more sophisticated by the day.
The rapid advancement of artificial intelligence in healthcare has ushered in a new era of diagnostic capabilities, yet the boundaries of AI diagnostic systems remain a subject of intense debate. While these technologies promise unprecedented efficiency and accuracy, their limitations and ethical implications cannot be overlooked. The conversation surrounding their application is as much about technological potential as it is about human responsibility.
The rapid proliferation of wearable devices has revolutionized how individuals monitor their health and fitness. From smartwatches tracking heart rates to fitness bands counting steps, these gadgets promise to deliver accurate and actionable data. However, as their usage expands into clinical research and medical applications, the question of data reliability becomes increasingly critical. How can we trust the numbers these devices generate? The answer lies in rigorous validation processes that ensure the accuracy and consistency of the data they produce.
The rapid advancement of telemedicine has transformed the way healthcare is delivered, particularly in the management of certain medical conditions. As the world becomes increasingly digital, healthcare providers and patients alike are recognizing the benefits of remote consultations. However, not all ailments are equally suited for virtual care. Identifying the appropriate conditions for telemedicine ensures efficiency, safety, and optimal patient outcomes.
The aviation industry has long recognized that the health and well-being of pilots are critical to ensuring flight safety. With thousands of lives in their hands every day, pilots must maintain peak physical and mental condition. Regulatory bodies worldwide have established stringent health management protocols to monitor and support pilots throughout their careers. These guidelines are not just about compliance—they represent a commitment to safeguarding both aviation professionals and the passengers who rely on their expertise.
The modern workforce has seen a significant rise in night shift workers, from healthcare professionals to factory operators and security personnel. These individuals operate on schedules that defy the body's natural circadian rhythms, leading to a host of physiological and psychological challenges. Understanding how to adjust their daily routines to better align with their unconventional hours is crucial for maintaining health, productivity, and overall well-being.
For vegetarians and vegans, ensuring adequate protein intake can sometimes be a challenge, particularly when it comes to obtaining all essential amino acids. Unlike animal-based proteins, which are complete proteins containing all nine essential amino acids, most plant-based proteins are incomplete. However, by combining different plant-based foods, vegetarians can create complete protein profiles that meet their nutritional needs.
The journey to full recovery after surgery is often a delicate process that requires careful attention to multiple factors, with nutrition playing a pivotal role. The body undergoes significant stress during surgical procedures, and the healing process demands an increased supply of essential nutrients. Without proper nutritional support, patients may experience delayed wound healing, weakened immunity, and prolonged recovery times. Understanding the relationship between diet and postoperative healing can make a substantial difference in a patient’s rehabilitation.
In the high-stakes world of competitive sports, maintaining peak physical condition is paramount. While much attention is paid to training regimens and nutrition plans, one critical aspect often overlooked is immune system maintenance. Athletes push their bodies to extremes, which can inadvertently weaken their immune defenses, leaving them vulnerable to illnesses that can derail training and competition schedules. A comprehensive immune maintenance program tailored for athletes is no longer a luxury—it’s a necessity.
As the global population ages, the importance of designing nutrient-dense meals for older adults has never been more critical. The concept of a "nutritionally dense plate" goes beyond simply providing calories—it focuses on maximizing essential vitamins, minerals, and other nutrients while minimizing empty calories. For seniors, whose metabolic needs and absorption capabilities change with age, this approach can significantly impact their overall health, mobility, and cognitive function.
Navigating the transition through menopause can be a challenging experience for many women, marked by a range of physical and emotional symptoms. While hormone replacement therapy (HRT) has long been a conventional approach, an increasing number of women are seeking non-hormonal alternatives to manage their symptoms. Whether due to personal preference, medical contraindications, or concerns about long-term risks, non-hormonal management strategies are gaining traction as viable options for symptom relief.
The adolescent years mark a critical period for skeletal development, where bones undergo rapid growth and mineralization. During this phase, physical activity plays a pivotal role in shaping bone density, strength, and overall structural integrity. However, not all exercises are created equal when it comes to optimizing bone health in teenagers. A well-designed exercise prescription must consider the unique physiological needs of growing bodies while minimizing injury risks.
Vision development in children is a complex and fascinating process that unfolds over several years. Unlike adults, children's visual systems are not fully mature at birth, and they undergo significant changes during early childhood. Understanding the key milestones in this developmental journey can help parents and caregivers ensure their child's eyesight is on track. From the first blurry weeks of life to the sharp clarity of school-age vision, each stage plays a crucial role in how children perceive and interact with the world around them.